The London Retina treatments
We deliver personalised and effective solutions for all aspects of eye health.
 Finance available
Finance available

My-iClinic ophthalmologists are medical doctors
Ophthalmology is the specialised field of medicine focused on the diagnosis, treatment, and management of eye disorders and diseases.
My-iClinic ophthalmologists are medical doctors who undergo extensive training to provide comprehensive eye care, from routine eye exams and prescription of corrective lenses to advanced surgical interventions.
They address a wide range of conditions, including cataracts, glaucoma, diabetic retinopathy, macular degeneration, and corneal diseases.
Our ophthalmologists employ cutting-edge technologies and surgical techniques to restore and preserve vision, ensuring the best possible outcomes for their patients.
Moreover, ophthalmologists work closely with optometrists and other eye care professionals to deliver personalised and effective solutions for all aspects of eye health.
Why my-iclinic
Comprehensive Care
My-iClinic ophthalmologists are equipped to handle a wide spectrum of eye care needs.
Advanced Techniques
We use cutting-edge technologies and surgical methods to ensure optimal results, aiming to restore and maintain vision to the highest standard.
Collaborative Approach
We collaborate with optometrists and other eye care professionals, ensuring a holistic, personalised solution for every aspect of eye health.




Yvonne Luo
Consultant and SurgeonYvonne Luo is an accomplished and highly skilled eye surgeon who brings her exceptional expertise to the esteemed team at My-iClinic in London.
With a stellar background in ophthalmology and a commitment to delivering the highest standard of eye care, Yvonne is a valuable asset to the clinic.
Her extensive training and experience encompass a wide range of eye conditions and surgical procedures, including cataract surgery, complex lens surgery, trauma repair , and treatments for various retinal disorders.
Yvonne's dedication to patient well-being, coupled with her innovative approach to eye care, ensures that individuals seeking top-tier ophthalmological services at My-iClinic receive comprehensive and compassionate care, underpinned by the latest advancements in the field.
Her presence at the clinic reinforces its reputation as a leading center for cutting-edge eye treatments and personalised patient care in the heart of London.Floaters
Floaters are black, or grey opacities in the vision.The commonest cause of floaters is due to the natural liquefaction of vitreous body with age.
This may be accompanied by flashing lights in the vision, a symptom of traction on the retina as the vitreous gel separates from the retina, a process known as posterior vitreous detachment.
While the process is innocuous most of the time, occasionally this can be associated with retinal tears, leading to retinal detachment (see below).
It is therefore imperative to have your eyes checked if you develop new flashing light and new floaters in your eyes, to ensure that the retina is intact and does not need urgent treatment. If the retina is intact, then treatment is usually not required.
While most of the patients grow accustomed to having floaters in the vision over time, some patients may find the floaters rather intrusive and distressing.
The most effective way of removing floaters is by a surgical procedure known as vitrectomy, whereby the vitreous jelly is liquefied by a high speed pneumatic cutter and removed, replacing it with clear balanced salt solutions, thereby effectively removing the opacities.



Retinal Detachment
Retinal detachment is a serious eye condition in which the retina, a thin layer of light-sensitive tissueat the back of the eye responsible for capturing light and sending visual signals to the brain, pulls away from its normal position.
This occurs when one develops a retinal tear during the posterior vitreous detachment. Once the retina is torn, fluid within the eye can seep through the break to accumulate underneath the retina, effectively separating it from the wall of the eye ball.
This separation can lead to a sudden and irreversible loss of vision if left untreated.
The primary procedure used to repair retinal detachment is called retinal re-attachment surgery.
There are several surgical techniques employed, including: vitrectomy, cryoretinopexy (localised freezing of retina tissue to allow adhesion of retina to the wall of the eyeball), laser retinopexy (localised laser of the retina to achieve adhesion to eyeball as above) with gas tamponade, scleral bucklingor a combination of these procedures.
Vitrectomy is a procedure in which the vitreous gel inside the eye is removed to get rid off the traction on the retina, and the retina is reattached by injecting a gas or oil bubble to push the retina back to its original positionand hold together with laser or cryotherapy.
Scleral buckling involves placing a silicone band around the eye to relieve the traction, allowing re-attachment of the retina to the wall of the eye ball with the help of cryoretinopexy.
The choice of procedure depends on the severity and location of the detachment.
Symptoms and signs of retinal detachment include new and sudden onset of flashing lights in either eye, new floaters in the eye, or a “shadow or curtain” effect from the periphery of your vision.
It is crucial to seek immediate medical attention if you suspect retinal detachment, as timely intervention can greatly improve the chances of preserving vision.


Macular Hole
A macular hole is a condition that affects the central part of the retina known as the macula, which is responsible for sharp and detailed central vision.
This disorder occurs when there is a small break or hole in the macular tissue, leading to distorted and blurred central vision.
Macular holes usually develop due to age-related changes of the vitreous body in eyes with abnormally strong adhesion of the vitreous at the macula.
As the vitreous body liquefies with age, the strong adhesion causes avulsion of the retinal tissue at macula, resulting in a macular hole.
Treatment of macular hole involves surgical procedures known as vitrectomy, peeling of internal limiting membrane, and gas tamponade.
During vitrectomy, the vitreous gel inside the eye is removed with a high speed pneumatic cutter and replaced with fluid. This removes all the traction on the retina.
A dye is then injected to stain a very thin connective tissue membrane on the surface of the retina, known as the internal limiting membrane.
By removing the (peeling away) the internal limiting membrane, the tissue around the macular hole becomes more mobile, and migrate to fill in the gap, thereby closing the macular hole. Finally, a gas bubble is injected to encourage migration of the surrounding tissue to fill the hole.
The visual outcome of the macular hole surgery is directly related to the size of the macular hole, which tends to enlarge with time.
Early diagnosis and prompt intervention are essential for achieving the best possible visual outcomes in macular hole cases.
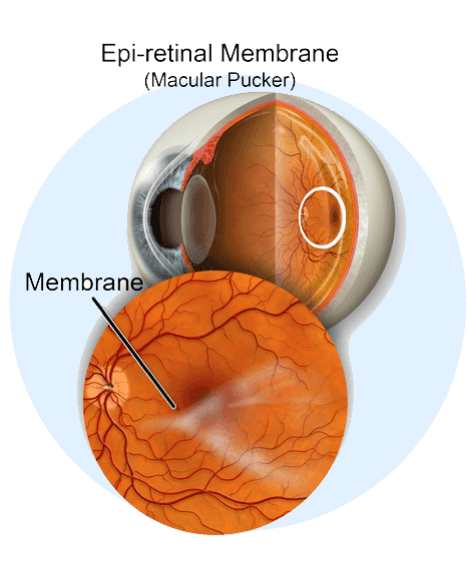
Epiretinal Membrane
Epiretinal membrane is a condition whereby a fibrotic tissue develops on the surface layer of the macula, the central part of retina responsible for fine detailed central vision.
As the fibrotic tissue contracts, it pulls on the underlying macula, resulting in distortion and blurring of the central vision, akin to someone physically wrinkling the film of a camera.
Epiretinal membrane is more commonly seen in patients who have diabetes, other ocular conditions such as previous retinal vein occlusions, previous retinal tears, but occasionally can occur in otherwise healthy eyes.
Treatment of epiretinal membrane involves surgically removing the jelly in the eyeball (vitrectomy), staining of the epiretinal membrane with a dye, then peeling away the fibrotic tissue away with forceps to relieve the traction on the underlying macula.
After the surgery, the retina usually takes up to 3 months to reorganise itself with an improvement of symptoms.


Diabetic Retinopathy
Diabetic retinopathy is a sight-threatening complication of diabetes that affects the blood vessels in the retina, the light-sensitive tissue at the back of the eye.
Over time, high levels of blood sugar can damage these delicate blood vessels, leading to leakage, swelling, and the development of abnormal blood vessels.
If left untreated, diabetic retinopathy can cause severe vision loss, including blindness.
The treatment for diabetic retinopathy varies depending on the stage and severity of the condition.
In the early stages, managing blood sugar levels, blood pressure, and cholesterol can slow its progression.
For more advanced cases, laser therapy (photocoagulation) or anti-VEGF injections may be recommended.
Regular eye examinations are crucial for early detection and management of diabetic retinopathy to preserve vision and prevent complications.
These treatments aim to reduce abnormal blood vessel growth and prevent further damage. In advanced cases, surgery such as vitrectomy may be necessary to remove blood or scar tissue from the eye.
Regular eye examinations are crucial for early detection and management of diabetic retinopathy to preserve vision and prevent complications.

Your eyesdeserve it.
World-class eye care with Yvonne Luo at My-iClinic in London.
Trust in Yvonne`s exceptional skills and commitment to excellence, and take the first step toward achieving optimal eye health and visual clarity.
Whether you're seeking...
Vision correction
Cataract surgery
Treatment for a complex eye condition
 Yvonne Luo
Yvonne Luo